Over the past three years, it has become clear that, for many people, the effects of SARS-CoV-2 infection persist long after an initial case of COVID-19 wanes.
Like primary COVID-19, the affliction, known as post-acute sequelae of SARS-CoV-2 (PASC) or long COVID, has highly variable duration, symptoms and severity. And as data accumulates, it appears that long COVID is a serious public health problem that will not go away any time soon.
There is still no widely accepted case definition for long COVID, but it generally refers to a range of persistent or new symptoms that remain present more than four weeks after the initial infection. In part because of the significant case-by-case disparities, it took the clinical community time to recognize it as a specific condition, but a code was implemented (“Post-COVID-19 condition”) for diagnosis on October 1, 2021. The code allows patients to be formally diagnosed with long COVID by a physician and the diagnosis to be entered into electronic health record (EHR) systems.
Jackson Laboratory Professor Peter Robinson, M.D., M.Sc., and Predoctoral Associate Ben Coleman have been investigating long COVID using EHR data from healthcare systems across the United States as part of the National COVID Cohort Collaborative (N3C). With the introduction of the diagnostic code, they and colleagues were able to analyze clinical data of patients diagnosed with long COVID to better define its characteristics. They also sought to determine whether it was possible to identify and define subtypes within the as-yet poorly understood umbrella diagnosis. Their findings, presented in “Generalisable long COVID subtypes: Findings from the NIH N3C and RECOVER programmes” and published in eBioMedicine, indicate that long COVID does indeed manifest in distinct subtypes that can help stratify patients and inform treatment strategies.
Long COVID subtypes
In all, Robinson and the team were able to obtain data for 20,532 patients who had received an official Post-COVID-19 condition diagnosis, from 38 data partners. While that number is very low—data for more than 5.4 million COVID-19 patients were in the N3C platform database by August 2022—the cohort is extremely important for long COVID research given that they all received diagnoses from a physician and they all have associated clinical data. The researchers defined long COVID as presenting 28 days after the earliest COVID-19 date noted for outpatients and 28 days after the end of hospitalization for inpatients.
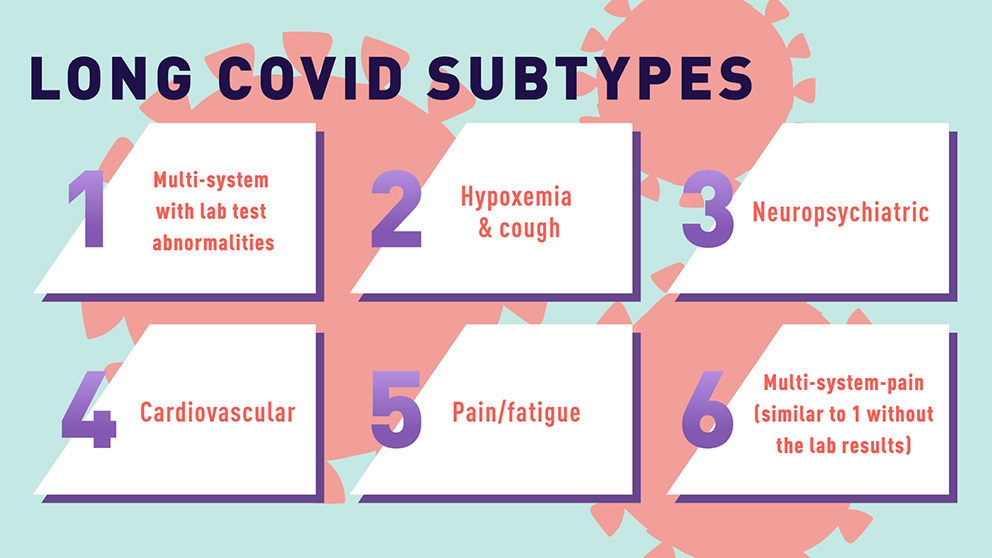
The team mapped the clinical findings to computable terms contained in the Human Phenotype Ontology (HPO), a standard framework for describing human traits that was developed and is maintained by the Robinson lab. This allowed the researchers to analyze the data across the entire cohort. After adapting a computational algorithm known as Phenomizer, they were able to determine a similarity metric between pairs of patients. Further calculations revealed the grouping of patients into six distinct clusters, each representing a different long COVID subtype. The subtypes are defined by the predominant clinical manifestations:
-
Multi-system + lab (associated with severe initial infection and a high frequency of multiple symptoms: neuropsychiatric, pulmonary, constitutional (e.g., general fatigue), cardiovascular, and vertigo as well as lab test abnormalities);
-
Hypoxemia and cough;
-
Neuropsychiatric (headache, insomnia, depression, movement abnormalities);
-
Cardiovascular;
-
Pain/fatigue; and
-
Multi-system-pain (similar to 1 without the lab results).
Each cluster has different age, gender and race frequencies associated with it, as well as different prior comorbidities and conditions.
Precision long COVID treatment
The findings underscore the possibility that the mechanisms of long COVID may vary among individuals based on a collection of baseline risk factors. In light of this, clinical research studies, such as the NIH’s “Researching COVID to Enhance Recovery (RECOVER),” will likely need to define sub-cohorts in their efforts to identify candidate therapeutics. And moving forward, stratifying long COVID patients will be important for effective treatment, as it is doubtful that any single approach will generalize well across the subtypes.